Prof. Josué Sznitman and his team from the Technion have developed an innovative technology that could dramatically improve the efficacy of existing drugs for treating Acute Respiratory Distress Syndrome (ARDS).
The technology could help save the lives of severe COVID-19 patients suffering from ARDS. Due to the global crisis, its development is being fast-tracked.
A research team led by Prof. Josué Sznitman of the Faculty of Biomedical Engineering at Technion is exploring the effectiveness of an innovative pulmonary treatment for ARDS, which is recognized as the leading cause of mortality in COVID-19 patients.
Sznitman and his team are in a race to launch clinical trials within a few months and evaluate the new technology for treating severe Coronavirus patients suffering from ARDS. To date, there is no existing therapy to treat ARDS patients. These patients undergo assisted ventilation and oxygenation, oftentimes under intubation, in intensive care units (ICUs).
One of the hallmarks of ARDS is damage to pulmonary surfactant (the liquid that coats the surface of alveoli in the lungs). Surfactant has many roles, but perhaps most importantly it reduces the forces required for breathing. While research is ongoing in understanding the SARS-COV-2 virus, it was recently shown that the virus kills the epithelial cells that secrete surfactant inside alveoli, after binding to a receptor (called ACE2) on the cell’s surface. Sznitman’s team hypothesizes that surfactant depletion may be particularly severe in COVID-19 related ARDS.
Surfactant Replacement Therapy (SRT) exists and is an established and life-saving clinical procedure in treating a similar type of ARDS that affects preterm newborn children, whose immature lungs lack pulmonary surfactant. In neonates, SRT is based on endotracheal administration of liquid surfactant (i.e. injecting external surfactant into the neonate’s lungs). As a result of differences in lung size, this delivery method has been highly ineffective in adults. Liquid instillations are strongly affected by gravity and thus quickly drain into pools, drowning some lung regions while leaving others entirely untreated.
The patent-pending technology, invented by Dr. Yan Ostrovski and Prof. Sznitman, and known as Liquid Foam Therapy (LIFT), is intended to dramatically improve the distribution of surfactant across the lungs. More generally, LIFT is a radical new method for pulmonary drug delivery with the potential of delivering therapeutics homogeneously into the lungs and, importantly in large doses. This is accomplished by loading the drug within the foam, or alternatively foaming the drug directly when possible. In both cases, and unlike liquids, the foam defies gravity and prevents the formation of pools.
In their findings (to be soon submitted for scientific publication and subject to rigorous peer-review), the team thoroughly examined in a preclinical in vivo study, the safety and efficacy of employing LIFT with foamed surfactant in a severe ARDS model induced in rats. There, the rats recovered a healthy state within 15-30 minutes, with no adverse events. As rat lungs are too small to demonstrate improved distribution that is critically sought in adult lungs, the team used ex vivo experiments in adult-sized porcine lungs to show how LIFT spreads homogenously compared with liquid administration.
Following these encouraging results, the team is now in a race to construct a fully functional delivery device and move to a preclinical in vivo study in severe ARDS models in pigs. If successful, the researchers will pursue the first clinical trials of the therapy, in an effort to critically accelerate the development of a treatment for the most severe COVID-19 patients with ARDS. The LIFT technology will be licensed to the newly founded start-up company, Neshima Medical, led by Dr. Ostrovski and supported by the Technion’s Business Development Unit T3.
Captions:
- Prof. Josué Sznitman
- Dr. Yan Ostrovski
- Prof. Sznitman (on the left) and Dr. Yan Ostrovski
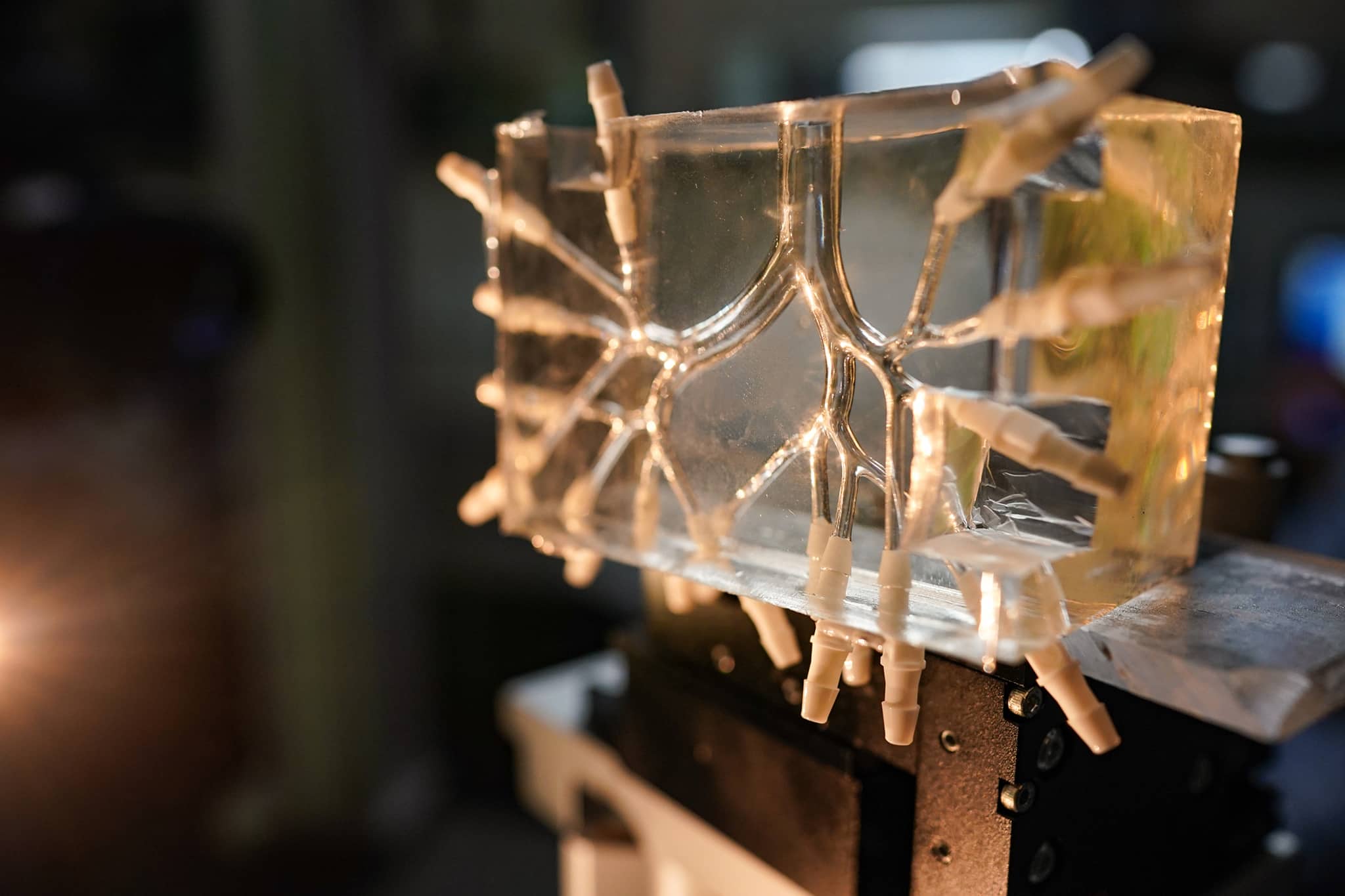
- The experimental setup – including a reconstructed upper airway “lung” model developed at the Technion
For addition information: Doron Shaham, Technion Spokesperson – 050-3109088